Women & Autoimmunity: Why We’re Prone to Medical Gaslighting
Alright, Autoimmune Thrivers; gather ‘round for a closer examination of a topic that resonates with many of us but is often overlooked: the complex connection between women and autoimmunity, and why our health issues are frequently dismissed as mere figments of our imagination, no thanks to what is commonly known as medical gaslighting. 😬
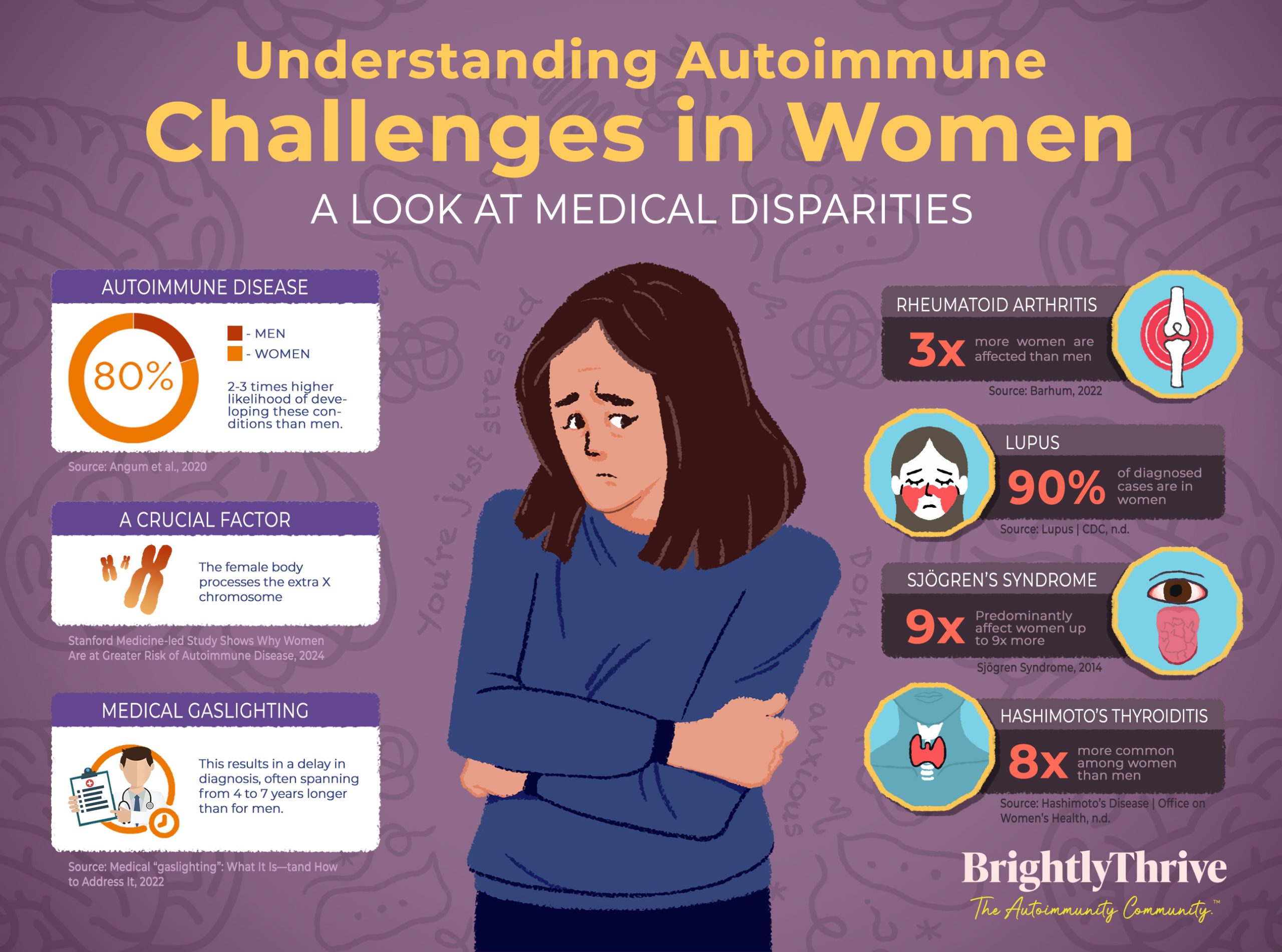
In the realm of autoimmune diseases, conditions where the body becomes its own adversary, a staggering 80% of those affected are women, with a two to three times higher likelihood of developing these conditions than men.
This isn’t just a matter of statistics; it’s about the genuine and unyielding challenges faced by women contending with diseases like Rheumatoid Arthritis, which affects three times more women than men, Lupus, diagnosed in 90% of cases in women, as well as Sjögren’s Syndrome and Hashimoto’s Thyroiditis, diseases that predominantly affect women up to nine and eight times more, respectively. Furthermore, recent research suggests the manner in which the female body processes the extra X chromosome could be a crucial factor.
And if that isn’t already distressing enough, the fight against these conditions is made even more difficult by the systemic obstacles of medical gaslighting, where symptoms are frequently brushed off as mere stress or anxiety, commonly experienced by women. This unfortunate reality results in an agonizing delay in diagnosis, often spanning from 4 to 7 years longer than for men. 🤯
What is Medical Gaslighting?
Imagine stepping into a world where your voice echoes back to you, unheard and unacknowledged. This is the realm of medical gaslighting, a shadowy corner of healthcare where the concerns of patients, particularly women, are minimized, dismissed, or labeled as figments of stress or anxiety. In this space, symptoms aren’t just symptoms; they’re often seen as overreactions, and pain is brushed off as “normal” or “imagined.” The result? A profound psychological and physical toll on those whose only wish is to be heard and healed.
Historical Background
The roots of this troubling phenomenon stretch deep into our history, tracing back to a time when women’s ailments were often dismissed under the catch-all diagnosis of hysteria (from which the word hysterical originated).
This antiquated term, originating from the Greek word for uterus, hystera, was used to explain a wide array of women’s health issues, effectively silencing their voices and medical needs. Already seeing the connection there? Such historical practices have left a lingering legacy in modern medicine, where biases and preconceptions continue to cloud the judgment of healthcare professionals, often at the expense of timely and appropriate care for women.
Modern-Day Challenges
But why does this matter so much, and why now? For women, especially in BIPOC (Black, Indigenous, and People of Color) communities, medical gaslighting isn’t just a personal grievance; it’s a systemic issue that perpetuates a dangerous cycle of neglect and disparity in healthcare.
The invisible symptoms of autoimmune diseases that many BIPOC individuals endure are often compounded by misunderstandings and stereotypes, further hindering their access to the necessary care.
Moreover, the manifestations of disease in these communities are frequently exacerbated by generational trauma and suppressed emotions, rooted in a culture that historically neglects their wellness.
There’s an urgent need for self-advocacy and proactive healthcare approaches within these communities, given the slow pace of change in medical understanding and practices. Culturally competent care becomes essential, which involves undoing the conditioning of being seen as the minority and advocating for oneself through education, assertive communication, seeking second opinions, requesting accommodations, and involving supportive allies in their care journey.
Yet, as we stand at this crossroads, peering into the abyss of challenges and inequities, there emerges a beacon of hope and solidarity. Communities like BrightlyThrive, The Autoimmunity Community™ and others, are weaving webs of connection, understanding, and advocacy.
Platforms such as ours are not just about sharing stories; they’re about changing narratives. They remind us that together, we possess the power to illuminate the darkest corners of healthcare, transforming whispers into roars for equity and compassion.
The Impact of Medical Gaslighting
Diagnosis Delays
For many women with autoimmune diseases, the journey to a correct diagnosis is longer and bumpier than it should be. This isn’t just inconvenient; it’s a critical period where untreated conditions can worsen, potentially causing irreversible damage, as in the case of Systemic Lupus Erythematosus (SLE) and many others. It’s unimaginable to wait for years, watching your health deteriorate, while desperately seeking answers. Unfortunately, this is the reality for far too many women. However, we cannot simply wait for the system to reset and fix itself. Surely, there must be ways for us to take ownership of our own healing and advocate for better healthcare.
Voices from our Community 💜
“I had a GI doc for a few months (very prestigious clinic with multiple referrals) that said he saw nothing abnormal on my GI endoscopy, but I had cut out gluten the week before the procedure. I told him I was feeling better and he said, “cutting out gluten won’t help you, you’re not celiac”. I remember feeling like a slap in the face and not feeling believed. I truly was feeling better! This was after a lifetime of going to doctors for pretty severe stomach pain and being told it was psychosomatic (aka all in my head): I no longer have stomach pain or acid reflux unless I eat gluten, so I find it very invalidating that I could have been feeling better for 22 years!” – Hanna Jade W.
The Emotional Weight of Being Dismissed
When your health concerns are brushed off as stress or imagination, the mental toll is heavy. This dismissal can lead to isolation, depression, and anxiety, as the very professionals you turn to for help seem to question your reality. But without giving up on the healthcare system and conventional medicine, how can we navigate the delicate balance of seeking integrative approaches and advocating for our own well-being without being sucked into an emotional whirlwind brought about by an autoimmune diagnosis?
Voices from our Community 💜
“When I was first getting symptoms of Crohn’s it took about half a dozen trips to the pediatrician before I was referred to a GI specialist. No tests were run, and my symptoms were branded “normal,” when they in fact were very abnormal. My condition progressed because of the lapse in care, which is frustrating to look back on. Later when I was dealing with a complication that was very painful, my GI doctor refused to prescribe pain medications even though I maxxed out on tylenol and it didn’t even touch me. I feel so betrayed and desperate.” – Alexa F.
Life Beyond the Waiting Room
The effects of delayed diagnosis stretch into every corner of life, from diminishing physical abilities to impacting work and social life. Every day spent waiting for answers is a day lost to potential relief and recovery.
But while time waits for no one, help is surely not too distant if we rely on others’ support and expertise to guide us through the journey towards diagnosis and treatment. Together, we can navigate the challenges of uncertainty and find solace in the knowledge and care provided by those who understand our struggles.
Systemic Issues Contributing to Medical Gaslighting
1. The Shadow of Implicit Bias
At the core of medical gaslighting lies the often-unseen force of implicit bias. These subconscious beliefs can shape the way healthcare professionals perceive and respond to women’s pain and symptoms, leading to a minimization of their experiences. It’s a pervasive issue that colors the medical encounter, sometimes leading practitioners to unconsciously downplay women’s health concerns or attribute them to emotional or psychological factors rather than physical ones. Recognizing and addressing these biases is crucial for creating a healthcare system that treats everyone’s concerns with the gravity they deserve.
2. Historical Context: The Ghost of “Hysteria”
 The historical treatment of women’s health issues casts a long shadow over modern medicine. From the 17th and 18th centuries, the diagnosis of “hysteria” served as a catch-all for a range of women’s physical and mental health conditions. Rooted in the belief that these ailments originated from the female reproductive system, the concept of a “wandering womb” or imbalances in female organs dominated medical explanations for women’s health issues.
The historical treatment of women’s health issues casts a long shadow over modern medicine. From the 17th and 18th centuries, the diagnosis of “hysteria” served as a catch-all for a range of women’s physical and mental health conditions. Rooted in the belief that these ailments originated from the female reproductive system, the concept of a “wandering womb” or imbalances in female organs dominated medical explanations for women’s health issues.
This legacy of dismissing women’s health concerns as overreactions or fabrications persists, contributing to the current climate of medical gaslighting. By understanding this historical backdrop, we can begin to see how deeply entrenched these attitudes are and the importance of actively dismantling them by raising awareness on the reality and impact of autoimmune diseases among women.
3. Lack of Research: A Gap in Knowledge and Care
A significant contributor to the issue of medical gaslighting is the gender disparity in autoimmune disease research funding. Despite women being disproportionately affected by autoimmune diseases, there’s a notable lack of research focused on understanding these conditions within the context of women’s health.
Case in point: Did you know that a study analyzing funding by the U.S. National Institutes of Health (NIH) found that diseases primarily affecting one gender are more likely to receive funding favoring males? This pattern is evident in nearly three-quarters of the cases, with diseases affecting more women often being underfunded relative to their disease burden.
This lack of research on female-dominant autoimmune diseases hinders our understanding of how these conditions manifest differently in women, potentially leading to misdiagnosis and a cycle of medical gaslighting. Bridging this research divide is essential for developing more effective diagnostic tools and treatments that can address the unique needs of women with autoimmune diseases.
Together, these systemic issues form a complex web that ensnares women’s voices, often leaving them unheard in the very places designed for healing. Addressing implicit bias, acknowledging historical missteps, and closing the research gap are critical steps toward dismantling the structures that perpetuate medical gaslighting. Through concerted efforts to understand and overcome these challenges, we can pave the way for a more inclusive and equitable healthcare experience for all women.
Steps for Change: Empowering Women and Transforming Healthcare
Embarking on a journey to transform healthcare for women with autoimmune diseases requires collective effort and individual empowerment. Here are some steps we can all take to advocate for change and support each other:
Patient Advocacy
- Educate Yourself: Dive into resources about autoimmune diseases. Websites, books, and patient forums can offer invaluable information. Don’t know where to start? BrightlyThrive™ offers exclusive on-demand resources within The Autoimmunity Community™ for our members, and bite-sized videos to increase your knowledge of living with autoimmune conditions and well-being tools for your healing journey.
- Be Assertive: Remember, you’re the expert on your own body. Don’t hesitate to express your concerns and ask questions during appointments.
Voices from our Community 💜
“I started to develop constant ringing in my ears (tinnitus) after a series of infusions for my autoimmune, when I sought help from my doctor, he simply said, “It’s probably nothing. Just try to ignore it. It will go away on its own” No advice, no support, just pure dismissal. Didn’t even look me in the eye or ask any follow-up questions! (I still have tinnitus to this day but have learned to manage it on my own thankfully!) It was a total wake-up call on the importance of self-advocacy in our health journeys. It reminded me that sometimes, we need to push HARD to be heard.”
– Noelle C.
- Seek Second Opinions: If something doesn’t feel right, it’s okay to consult another healthcare provider. A fresh perspective can make all the difference.
Physician Education
- Implicit Bias Training: Encourage healthcare institutions to incorporate implicit bias training. It’s essential for creating a more inclusive healthcare environment.
- Improve Communication: Workshops on effective communication can help healthcare professionals better understand and connect with their patients.
- Continuing Education: Support and advocate for programs that keep healthcare professionals up to date on the latest in autoimmune disease research and treatment options.
Increased Research
- Advocate for Funding: Funding for women’s health research, particularly for autoimmune diseases, is crucial for better diagnosis and treatment. Here’s how you can make a difference:
- Contact Your Representatives: Find your local representatives’ contact information online and send a quick email or letter expressing your support for increased funding for women’s health research.
- Support Advocacy Organizations: Many organizations work tirelessly to raise awareness and secure funding for autoimmune diseases. Research and consider donating to groups like the National Institutes of Health (NIH) or the Autoimmune Association (formerly known as the American Autoimmune Related Diseases Association).
- Participate in Studies: Getting involved in clinical trials or research can make a significant difference. Your participation could pave the way for new discoveries in the treatment and understanding of autoimmune diseases. Here’s how you can make an impact:
- Stay Informed: Keep an eye on websites and newsletters from reputable health organizations on upcoming studies.
- Connect with Specialists: Ask your healthcare provider about any known clinical trials or research projects looking for participants.
- Use Clinical Trial Finders: Online platforms and databases are available to help you find studies that match your condition and preferences.
- Understand the Commitment: Before signing up, make sure you understand what participation involves and how it might impact your schedule and health.
Your role in these studies is more than participation; it’s a contribution to a future where autoimmune diseases are better understood and more effectively treated.
- Raise Awareness: Your journey and voice have the power to illuminate the need for deeper research into autoimmune diseases. By sharing your experiences on social media and community platforms, you become a beacon of awareness. Here’s how you can make a profound impact:
- Embrace Your Narrative: Your personal story is unique and can resonate deeply with others. Share your challenges and triumphs in navigating autoimmune diseases.
- Foster Empathy: When discussing these topics, gently remind your audience about the importance of understanding and empathy. Your approach can encourage compassionate conversations.
- Engage with Purpose: Use your platforms not just to share, but to educate and inspire action. The more we collectively understand, the stronger our call for necessary research funding.
Remember, your voice is a powerful tool for change. By owning your story and engaging with others empathetically, you help build a community that’s informed, supportive, and motivated to advocate for advancements in autoimmune disease research.
Community Support
- Tap Into Online Communities: Leverage the power of online forums and platforms like the BrightlyThrive™ Community. These spaces offer not just support and advice, but also a sense of belonging. When you share your journey, you open the door for others to do the same, creating a ripple effect of inspiration and solidarity.
- Create a Support Group: Initiating a support group (for some, a.k.a ladies lunch), be it virtually or in your local community, cultivates a sanctuary for women to exchange insights and strategies for managing healthcare challenges. This act of gathering can transform individual struggles into collective strength.
- Spread Awareness Among Loved Ones: Use your voice to enlighten friends and family about autoimmune diseases and the power of advocacy. Change often sprouts from the soil of our own communities, growing outward from the understanding and support of those we hold dear.
At the core of our community efforts, BrightlyThrive™ cultivates a space where no one navigates their health journey in isolation. Instead, we come together as a vibrant network, rich in social connections, that actively enhances our understanding of autoimmune diseases and celebrates the unique stories each of us brings to the table. Here, every individual is an integral thread in a tapestry of shared experiences and collective wisdom, empowering us to face our challenges with strength and unity.
ThriveGuide™ Insights

Recently, Christina Tildwell, one of our esteemed ThriveGuides™ and a registered nurse, shared invaluable insights into How to Make the Most of Your Doctor’s Visits within our community. Like many of us, Christina has navigated the all-too-common feeling of being rushed and unheard during medical appointments as a patient herself.
Her journey, however, also highlights a brighter side—a testament to those healthcare professionals who invest time and genuine care in understanding their patients’ health narratives.
Through Christina’s experience, we’re reminded that, while finding such dedicated practitioners may seem daunting, they do exist, and it’s possible to forge meaningful partnerships in our healthcare journeys.
Christina’s contribution goes beyond sharing personal anecdotes; she offers tangible strategies to enhance our interactions with healthcare providers. During her Thrive Live, she revealed practical tools, including her very own Appointment Checklist designed to empower us to take charge of our healthcare conversations.
This checklist is a powerful resource for anyone seeking to be fully seen and heard, ensuring no detail of their health story is overlooked. Christina’s wisdom underscores the possibility of turning every doctor’s visit into an opportunity for deeper understanding and collaboration, regardless of the complexity of our health concerns, autoimmune-related or otherwise.
Christina shared: “It’s vital to be proactive during these visits. Had I not prepared my questions, I would have been flustered and stressed. After my visit, I jotted down the answers to ensure I wouldn’t forget them. It’s also useful to have someone accompany you during your visit. They can provide a second set of ears or help take notes. Getting a diagnosis or discussing your health can sometimes be stressful, causing us to forget, so having someone else there can be incredibly helpful.”
Joining BrightlyThrive™ not only connects you with Christina’s insights but also opens the door to a wealth of resources and a supportive network committed to navigating the healthcare system more effectively. As a community, we’re dedicated to transforming the narrative around healthcare visits from one of frustration to one of empowerment and partnership.
Empowering the Journey: Transforming Women’s Health and Autoimmunity Together
Navigating the complexities of women’s health and autoimmunity reveals a path filled with challenges, yet it’s paved with the promise of transformation and unity. As we shed light on the shadows of medical gaslighting, our collective journey emphasizes the power of education, assertiveness, and community.
By championing patient advocacy, enhancing physician understanding, pushing for targeted research, and nurturing supportive networks, we’re not just confronting systemic barriers; we’re crafting a future where every woman’s health concern is met with empathy and action.

Resources
Invernizzi, P., Pasini, S., Selmi, C., Gershwin, M. E., & Podda, M. (2009, August). Female predominance and X chromosome defects in autoimmune diseases. Journal of Autoimmunity, 33(1), 12–16.
Kronzer, V. L., Bridges, S. L., & Davis, J. M. (2020, December). Why women have more autoimmune diseases than men: An evolutionary perspective. Evolutionary Applications, 14(3), 629–633.
Arthritis and Sjögren’s Syndrome. (2003, December 3). WebMD.
Rheumatoid arthritis. (2023, June 28).
Barber, M. R. W., Drenkard, C., Falasinnu, T., Hoi, A., Mak, A., Kow, N. Y., Svenungsson, E., Peterson, J., Clarke, A. E., & Ramsey-Goldman, R. (2021, August 3). Global epidemiology of systemic lupus erythematosus. Nature Reviews Rheumatology, 17(9), 515–532.
Mariette, X., & Criswell, L. A. (2018, March 8). Primary Sjögren’s Syndrome. New England Journal of Medicine, 378(10), 931–939.
Mincer, D. L., & Jialal, I. (2023, July 29). Hashimoto Thyroiditis. StatPearls – NCBI Bookshelf.
Neergaard, L. (2024, February 1). Lupus and other autoimmune diseases strike far more women than men. Now there’s a clue why | AP News. AP News.
How to navigate “medical gaslighting” when doctors dismiss your symptoms. (2022, March 14). TODAY.com.
Cook, R. (2022, May 12). What BIPOC need to know about Medical Gaslighting — The Grapevine. The Grapevine.
Sabin, J. A. (2022, July 14). Tackling Implicit Bias in Health Care. New England Journal of Medicine, 387(2), 105–107.
Gershon, L. (2021, June 8). Myth and Misdiagnosis Have Plagued Women’s Health for Centuries. Smithsonian Magazine.
Mirin, A. A. (2021, July 1). Gender Disparity in the Funding of Diseases by the U.S. National Institutes of Health. Journal of Women’s Health, 30(7), 956–963.
TAGS:
CATEGORIES: