Understanding Your Body: The Menstrual Cycle’s Role in Perimenopause
Imagine for a moment that your body is a masterpiece, a symphony of biological wonders playing in perfect harmony. It’s the same body that can create life, nourish it, and now, as you approach perimenopause, it’s tuning itself to a new rhythm.
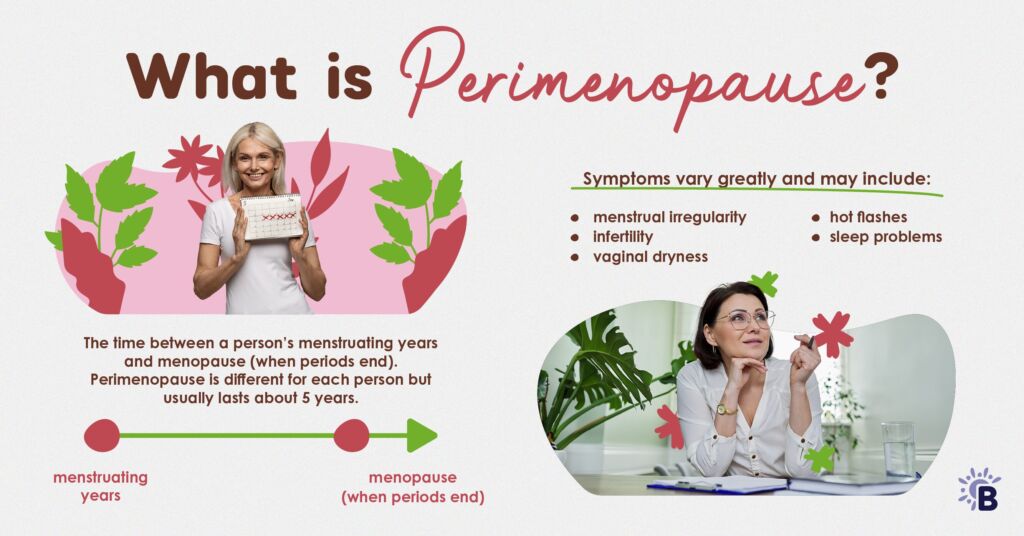
Perimenopause is not just a biological shift; it’s a powerful transition in the life of every woman, where understanding the subtle changes in your menstrual cycle can unlock a new level of self-awareness and strength.
Just as you once marveled at the miracle of childbirth or the nurturing connection of breastfeeding, you can now embrace this phase with the same awe and appreciation, recognizing it as yet another chapter in the story of your body’s incredible capabilities.
The Menstrual Cycle and Hormonal Phases
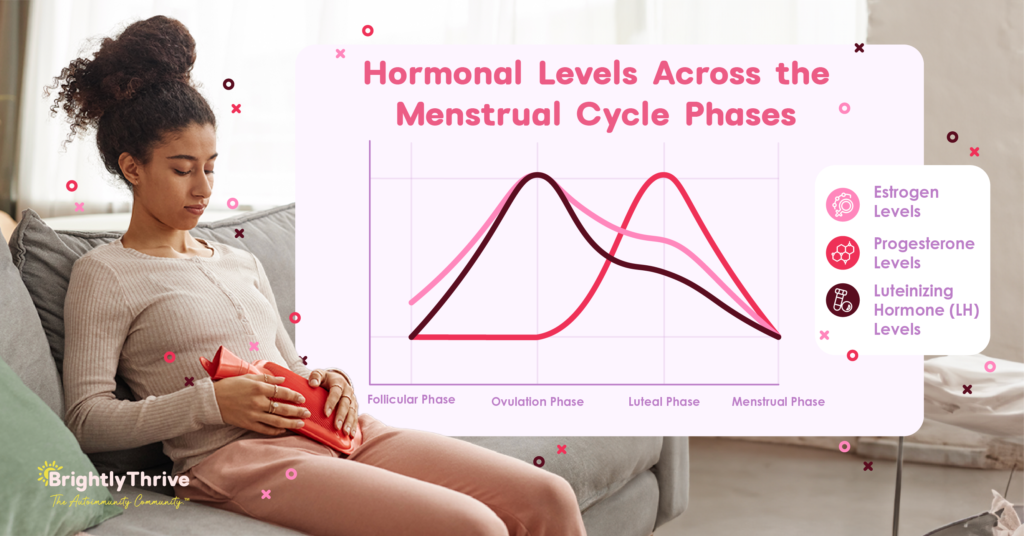
The menstrual cycle, regulated by hormones, is divided into four phases:
- follicular,
- ovulation,
- luteal, and
- menstrual.
Each phase influences not just reproductive health but overall well-being. During perimenopause, these hormonal patterns become less predictable, leading to symptoms like irregular periods and mood swings.
For women with autoimmune conditions, these fluctuations can significantly impact symptom severity, as hormonal shifts, particularly in estrogen, may either alleviate or exacerbate autoimmune symptoms. Understanding these interactions is key to managing both perimenopausal and autoimmune (AI) symptoms effectively.
Follicular Phase: The Fresh Start
- Hallmark: Rising estrogen levels.
- Key Characteristics: Begins on the first day of menstruation and lasts until ovulation. This phase is marked by the growth of follicles in the ovaries, preparing for the release of an egg.
- Cognitive improvements, better mood, and increased energy are common during this phase.
- Implications for AI health: During the follicular phase, you may feel more focused and energized, making it a good time for complex tasks and social activities. However, due to the unpredictability of perimenopause, avoid overexertion. Maintain a balanced routine with gentle exercise, a healthy diet, and stress management to support your well-being and manage autoimmune symptoms effectively.
- Perimenopause Impact: Ovulation may become irregular, leading to unpredictability in the benefits typically associated with this phase.
Ovulation Phase: The Peak of Fertility
- Hallmark: Peak in estrogen and luteinizing hormone (LH) surge.
- Key Characteristics: Occurs mid-cycle when the mature egg is released from the ovary.
- This phase is associated with heightened fertility, increased libido, and enhanced verbal and communication skills.
- Implications for AI health: Take advantage of this period for social interactions but stay mindful of potential symptom changes. Prioritize self-care and avoid overcommitting to maintain balance and manage your health effectively.
- Perimenopause Impact: Even if ovulation is irregular, the hormonal surge still occurs, which can affect libido and mood, as well as impact autoimmune symptoms.
Luteal Phase: Preparing for the Next Cycle
- Hallmark: Rising progesterone and declining estrogen levels.
- Key Characteristics: After ovulation, the body prepares for a potential pregnancy.
- This phase can bring enhanced fat metabolism, increased exercise endurance, and heightened emotional sensitivity.
- Implications for AI health: This is a good time to focus on moderate exercise to take advantage of improved endurance, but be cautious not to overdo it, as fluctuations in hormone levels could worsen symptoms. Prioritize activities that promote emotional balance, like yoga or meditation, and consider adjusting your diet to support fat metabolism while avoiding triggers that could exacerbate autoimmune flare-ups.
- Perimenopause Impact: Fluctuations in hormone levels can lead to variability in symptom severity, particularly for women with autoimmune conditions.
Menstrual Phase: The Cycle Restarts
- Hallmark: Low levels of estrogen and progesterone.
- Key Characteristics: This phase is marked by menstruation, as the lining of the uterus is shed.
- It’s a time of hormonal reset and physical cleansing.
- Implications for AI health: Focus on self-care by incorporating gentle activities like walking or stretching to manage discomfort. Ensure your diet is rich in anti-inflammatory foods and prioritize rest to support your body through this cleansing phase. Be mindful of stress levels, as hormonal drops can make your body more susceptible to autoimmune reactions, making this an essential time for self-care.
- Perimenopause Impact: Menstrual cycles can become irregular, with lighter or heavier bleeding. The drop in hormone levels can also exacerbate autoimmune symptoms, making self-care crucial.
The key to thriving with autoimmunity during perimenopause is understanding how hormone shifts affect your symptoms. The common thread? Estrogen and progesterone levels. Stay in tune with these changes, adjust your routine, focus on an anti-inflammatory diet, and manage stress. These simple steps can help you navigate flare-ups and maintain your well-being through this transition.
The good news is that you don’t have to go through this season alone. At BrightlyThrive, The Autoimmunity Community™, you can get personalized support, expert guidance, and a community that understands your journey and phases in your autoimmune life. Together, we’ll help you thrive. Become a member today.
Conclusion
Tuning into your body’s changes during perimenopause, especially when managing autoimmune conditions, is vital. By recognizing the benefits and challenges of each phase, women can navigate this life stage with resilience and strength, finding empowerment in our body’s incredible capacity for change.
References
Desai, M. K., & Brinton, R. D. (2019). Autoimmune Disease in Women: Endocrine Transition and Risk Across the Lifespan. Frontiers in endocrinology, 10, 265.
https://doi.org/10.3389/fendo.2019.00265
How Does Perimenopause Affect Your Periods?: Solace Women’s Care: Obstetrics & Gynecology. (n.d.-b). https://www.solacewomenscare.com/blog/how-does-perimenopause-affect-your-periods
McCarthy, M., & Raval, A. P. (2020). The peri-menopause in a woman’s life: a systemic inflammatory phase that enables later neurodegenerative disease. Journal of Neuroinflammation, 17(1). https://doi.org/10.1186/s12974-020-01998-9
The menstrual cycle. (n.d.). Better Health Channel. https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/menstrual-cycle
HealthCentral. (n.d.). Menopause and autoimmune disease. https://www.healthcentral.com/article/menopause-and-autoimmune-disease
TAGS:
CATEGORIES:





