
Dream Hospital: The Future of Healthcare We Envision
Healthcare today faces a myriad of challenges, from impersonal environments that can leave patients feeling isolated and anxious, to a system that often prioritizes treatment over prevention. These limitations highlight a significant gap between the current state of hospitals and the ideal healing environment many of us envision. And here is where the concept of the “dream hospital” comes in. This is not just a whimsical fantasy, but a tangible goal that embodies innovation, patient-centered care, nutrition, environmental sustainability, and holistic wellness.
This dream hospital represents a radical departure from traditional healthcare settings, proposing a future where healing spaces are vibrant, food serves as medicine, and care is comprehensive and holistic. In exploring this vision, we not only imagine what could be but also set a new standard for what should be in the evolution of healthcare.
Join us as we delve into the collective vision of our BrightlyThrive™ community members, as they picture out the healthcare that we all truly deserve. With the assistance of AI technology, we transformed their ideas into artistic imagery and gained a new perspective on how healthcare should evolve in the future.
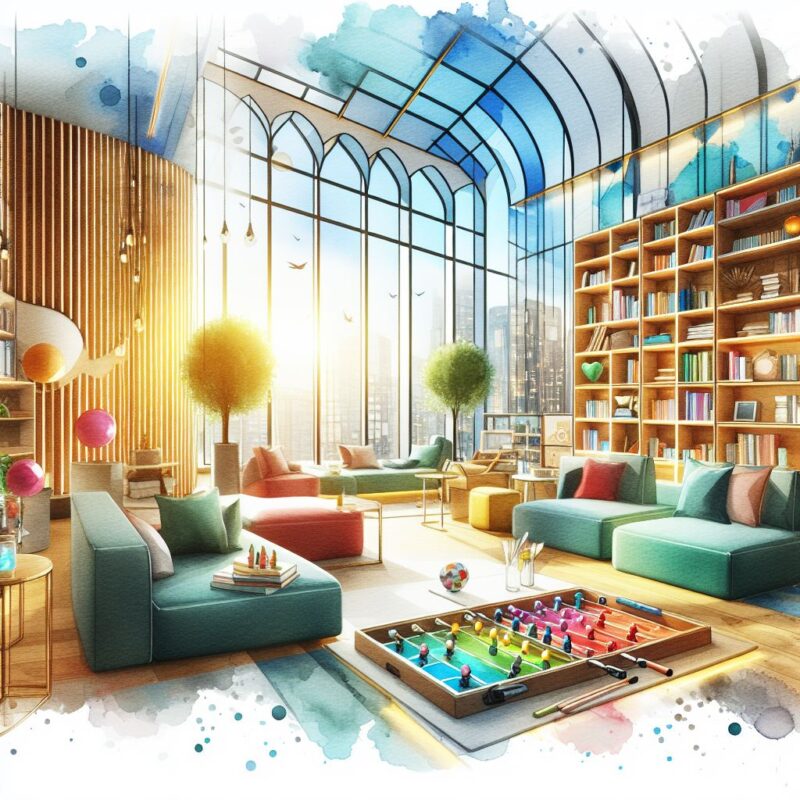
1. A Vibrant and Healing Environment
The design and atmosphere of a hospital significantly impact patient recovery, emphasizing the need for environments that promote both physical and emotional well-being.
- Colorful Spaces: Research suggests that bright and cheerful colors can positively affect mood and reduce stress, making them a vital component of hospital design. These hues can transform spaces into welcoming environments that encourage optimism and vitality, crucial for patient recovery.
- Connection with Nature: The inclusion of green outdoor spaces and gardens is supported by studies highlighting the benefits of nature on mental health, including stress reduction and improved mood. Access to these areas allows patients and their families to experience tranquility and rejuvenation, which are essential for holistic and autoimmune healing.
- Therapeutic Interactions with Animals: Animal-assisted therapy has been shown to decrease pain and anxiety in patients, supporting the incorporation of therapeutic petting zoos as a novel approach to care.
2. Nutrition and Nourishment
- The Role of Food in Healing: Research underscores the profound impact of nutrition on healing and recovery. A hospital that employs nutritionists and chefs specializing in nutrient-dense diets, such as the paleo diet, recognizes the scientific evidence linking diet quality to improved patient outcomes. Nutrient-dense foods, characterized by their rich content of vitamins, minerals, and antioxidants, have been shown to support immune function, enhance wound healing, and reduce inflammation, accelerating the recovery process.
- A Fresh Approach to Hospital Meals: The integration of fresh, whole foods into hospital menus represents a significant shift towards prioritizing patient health and wellness. Scientific studies advocate for the consumption of fresh produce and high-quality proteins to not only aid in recovery but also improve the overall quality of life.
This approach aligns with the growing body of evidence suggesting that diets rich in fresh fruits, vegetables, and lean meats can have a positive impact on health outcomes, including reducing the risk of chronic diseases and supporting mental health.

3. Holistic and Integrative Care
- Comprehensive Wellness Teams: Research underscores the importance of multidisciplinary teams in healthcare, demonstrating that collaborative care models can lead to better patient outcomes, higher patient satisfaction, and reduced healthcare costs. By integrating the expertise of therapists, health coaches, and somatic practitioners alongside traditional medical staff, patients receive care that is more personalized, proactive, and preventive.
- Wellness Tools and Therapies: Evidence-based practices such as acupuncture, massage therapy, and light therapy have been shown to effectively complement conventional medical treatments. For instance, acupuncture and massage therapy are recognized for their pain-relieving effects and role in reducing post-operative pain and chronic pain conditions. Similarly, red light therapy has been found to promote wound healing, reduce inflammation, and improve skin conditions.
Integrating these therapies into patient care not only addresses physical symptoms but also supports mental and emotional well-being, contributing to a more holistic recovery process.

4. Rest, Recovery, and Recreation
- Self-Care and Rest Areas: Research underscores the critical role of rest and mental well-being in the recovery process. In envisioning the future of healthcare, it’s essential to incorporate dedicated spaces for self-care and rest, as these environments significantly contribute to reducing stress and improving patient outcomes. Meditation and relaxation spaces, supported by studies, enhance mental health by lowering anxiety and improving coping mechanisms during treatment and recovery.
- Engaging Activities for Connection: Additionally, the importance of social support and engaging activities in healing is well-documented. Spaces designed for patients and families to engage in activities together not only provide emotional support but also have been shown to improve the overall hospital experience. Positive interactions and shared experiences contribute to better emotional well-being, which is linked to faster recovery rates.

At BrightlyThrive, The Autoimmunity Community™, we prioritize social support and engaging activities to enhance our members’ autoimmune healing journeys. Through virtual events, quarterly challenges, and shared experiences, we foster connections and uplift one another. Join us at BrightlyThrive™ and let’s thrive together!
5. Staffing and Support
- Valuing Healthcare Workers: Did you know that there’s a critical link between the well-being of healthcare workers and the quality of patient care? Well-rested, adequately resourced, and validated staff are fundamental to delivering compassionate and efficient healthcare. Evidence shows that supporting healthcare professionals not only enhances patient outcomes but also reduces burnout, a significant barrier to care quality.
- Educational Workshops and Events: Educational programs on holistic living and nutrition for staff have been shown to improve patient care by integrating comprehensive wellness approaches into traditional medical practices. Such initiatives also contribute to a culture of continuous learning and job satisfaction among healthcare workers, ultimately fostering a more effective and empathetic healthcare environment.

Presenting the Dream Hospital – A New Horizon in Healthcare

The “dream hospital” concept presents a revolutionary vision for healthcare, emphasizing the need for a system where innovation meets compassion and holistic, patient-centered care becomes the norm. We can all agree that while ambitious, these ideals are essential for fostering a healthcare environment that prioritizes comprehensive wellness for both patients and providers. This vision compels us to advocate for and implement changes that resonate with our deepest values of care, ensuring a healthier future for generations to come.
Resources
Dalke, H., Little, J., Niemann, E., Camgoz, N., Steadman, G., Hill, S., & Stott, L. (2006, June). Colour and lighting in hospital design. Optics & Laser Technology, 38(4–6), 343–365.
The wellness benefits of the great outdoors | US Forest Service. (n.d.). US Forest Service.
López-Fernández, E., Palacios-Cuesta, A., Rodríguez-Martínez, A., Olmedilla-Jodar, M., Fernández-Andrade, R., Mediavilla-Fernández, R., Sánchez-Díaz, J. I., & Máximo-Bocanegra, N. (2023, November 8). Implementation feasibility of animal-assisted therapy in a pediatric intensive care unit: effectiveness on reduction of pain, fear, and anxiety. European Journal of Pediatrics, 183(2), 843–851.
Clinic, C. (2024, March 29). What To Eat When You’re Trying to Heal. Cleveland Clinic.
Downer, S., Berkowitz, S. A., Harlan, T. S., Olstad, D. L., & Mozaffarian, D. (2020, June 29). Food is medicine: actions to integrate food and nutrition into healthcare. BMJ, m2482.
Singer, J., & Adams, J. (2014, May 22). Integrating complementary and alternative medicine into mainstream healthcare services: the perspectives of health service managers. BMC Complementary and Alternative Medicine, 14(1).
Wu, M. S., Chen, K. H., Chen, I. F., Huang, S. K., Tzeng, P. C., Yeh, M. L., Lee, F. P., Lin, J. G., & Chen, C. (2016, March 9). The Efficacy of Acupuncture in Post-Operative Pain Management: A Systematic Review and Meta-Analysis. PLOS ONE, 11(3), e0150367.
Wu, M. S., Chen, K. H., Chen, I. F., Huang, S. K., Tzeng, P. C., Yeh, M. L., Lee, F. P., Lin, J. G., & Chen, C. (2016, March 9). The Efficacy of Acupuncture in Post-Operative Pain Management: A Systematic Review and Meta-Analysis. PLOS ONE, 11(3), e0150367.
Professional, C. C. M. (n.d.). Red Light Therapy. Cleveland Clinic.
Mindfulness meditation: A research-proven way to reduce stress. (2019, October 30). https://www.apa.org.
How Does Social Connectedness Affect Health? (2023, May 8). Centers for Disease Control and Prevention.
Teoh, K., & Hassard, J. (2020). Linking Organisational Factors and Patient Care: Does Healthcare Workers’ Well-being Matter? Connecting Healthcare Worker Well-Being, Patient Safety and Organisational Change, 41–57.
Sassen, B. (2023). Nursing and Holistic Care. Improving Person-Centered Innovation of Nursing Care, 1–10.
TAGS:
CATEGORIES:







